The Provider Enrollment and Management System (PEMS) fully deployed on December 13, 2021. The system introduced new business rules for enrollment in Texas Medicaid.
Prior to the PEMS implementation, the provider billing effective date could be either the Medicare enrollment effective date, the provider license date, or the application completion date (retroactive billing date).
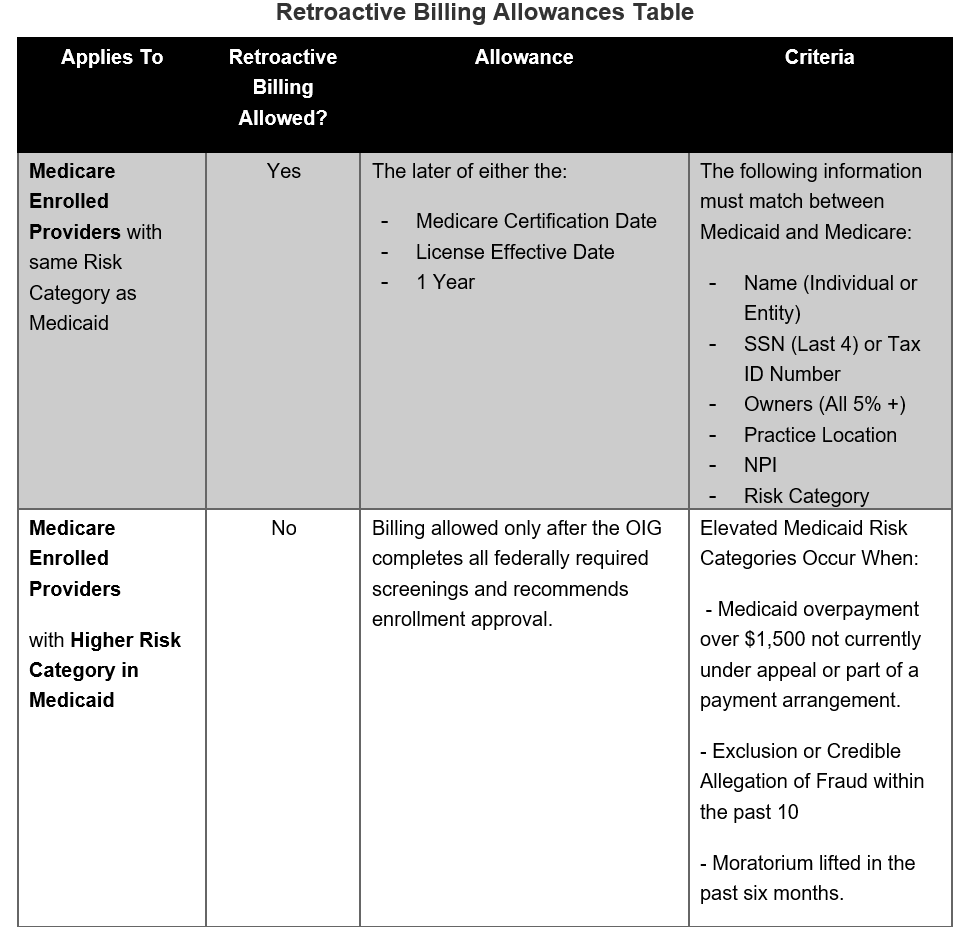
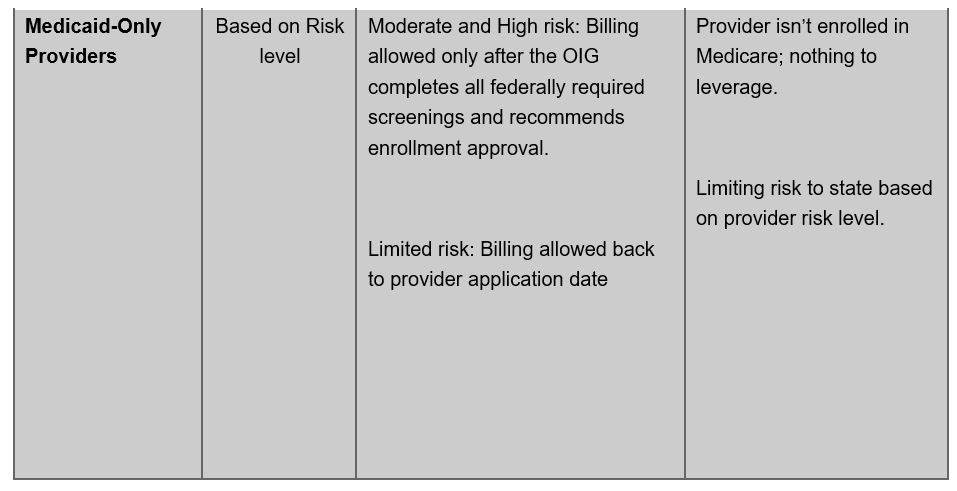
With PEMS implementation, new and reenrolled provider agreement effective dates were upon signature of the agreements and required all screenings to be completed. After further review, HHSC, in collaboration with the Office of Inspector General (OIG) made the decision to allow retrospective billing effective dates in certain circumstances, as outlined in the table below. The new policy applies to new enrollments and reenrollments only.
The retroactive effective date appeared on the master provider file starting July 5, 2022. HHSC has directed Texas Medicaid & Healthcare Partnership to reprocess denied claims for providers. HHSC directs MCOs to allow for the reprocessing of claims for providers with the retroactive billing effective dates.
More information on PEMS can be found at Provider Enrollment | TMHP
Please find the Retroactive Billing Allowances table below.
For assistance, please contact Community First Provider Relations:
Email: ProviderRelations@cfhp.com | Phone: (210) 358-6294