Personal Care Services (PCS) is considered medically necessary when a member requires help with activities of daily living (ADLs), instrumental activities of daily living (IADLs), or health maintenance activities (HMAs) because of physical, cognitive, or behavioral limitation related to the member’s disability or chronic health condition. The member’s disability or chronic condition must be substantiated by a Practitioner’s Statement of Need (PSON). A signed PSON is required annually and for a significant change in condition.
PROCESS
- CFHP Staff fax a request to member’s practitioner when PCS is requested.
- Generate fax request with subject line: ***URGENT REQUEST***
- In the body of the message, include the statement below:
- Hello Practitioner, Please complete Sections A-E of the Provider Statement of Need form for this member. Once completed with signature and date, please fax back to CFHP at 210-358-6274 or email to designated CFHP staff (will be identified on fax cover sheet) in order to begin or continue to authorize Personal Care Services. If you have any questions, call Community First at 210-358-6403. Thank you.
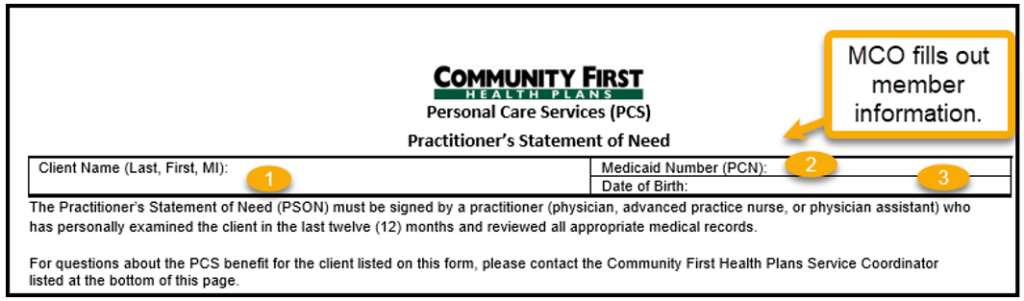
2. The PSON member information is completed by CFHP staff, to include Client name, Medicaid number and Date of Birth.
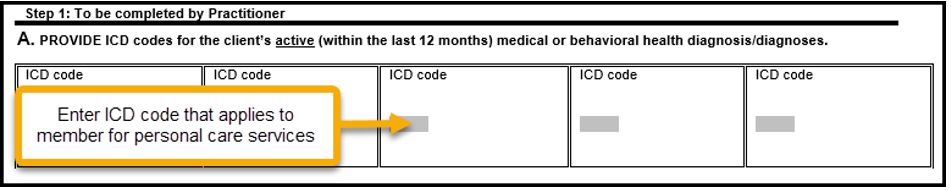
3. Step 1: To be Completed by Practitioner.
- Section A: Provide ICD codes for the client’s active medical or behavioral health diagnosis/diagnoses. Active diagnoses include any diagnosis requiring treatment in the last 12 months.
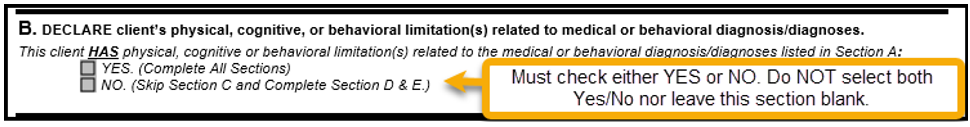
- Section B: Declare client’s physical, cognitive, or behavioral limitation(s) related to medical or behavioral diagnosis/diagnoses. This client HAS physical, cognitive, or behavioral limitation(s) related to the medical or behavioral diagnosis/diagnoses listed in Section A. Select either YES or NO. Do NOT leave this section blank.
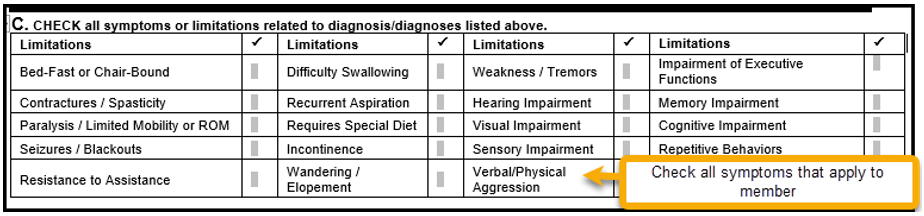
- Section C: CHECK all symptoms or limitations related to diagnosis/diagnoses listed in section A.
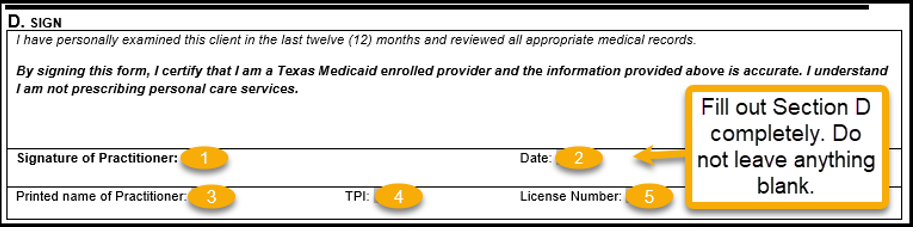
- Section D: Sign. This certifies that client has been examined in the last 12 months and medical records reviewed. The practitioner also certifies they are a Texas Medicaid enrolled provider. The practitioner does not prescribe personal care services.
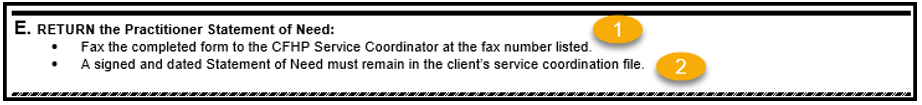
- Section E: Return the Practitioner Statement of Need
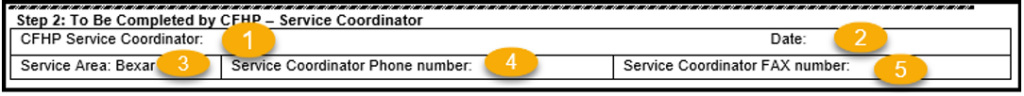
4. Step 2: To be Completed By CFHP – Service Coordinator.