Effective for dates of service on or after February 1, 2022, Autism Services, to include Applied Behavior Analysis (ABA) evaluation and treatment, will be a benefit of the Texas Health Steps-Comprehensive Care Program (THSteps-CCP) for Texas Medicaid recipients who are 20 years of age and younger and who meet the criteria outlined in the Autism Services Benefit description.
Beginning February 1, 2022, HHSC will be implementing three new business edits that are specific to encounter data submission for Medicaid Autism services. These encounter data business edits enforce policy for billing, and reimbursement for procedure codes 97151, 97153, 97154, 97156, 97158, and 99366.
Autism services are reimbursed in accordance with 1 Texas Administrative Code § 355.
If services billed exceed the limitations outlined in this policy, the claim will be denied or rejected. The medical encounter must include diagnosis code F84.0 (Autism disorder) in any diagnosis position. This benefit is available for members age 0-20 years old. Claims submitted for members over 20 years of age may be denied or rejected.
Providers are required to submit their NPI in the enrollment application. During the enrollment process, providers must also select a primary, and if applicable, secondary taxonomy codes associated with their provider type. Providers must verify the taxonomy codes associated with their provider type and specialty before beginning the enrollment process. Providers submitting claims for these services should enroll with provider specialty 51 and provider type 86. Failure to submit claims with the correct taxonomy code, 103K00000X, could result in claims being denied or rejected.
Direct treatment for the child/youth is limited to a total of 8 hours per day, inclusive of procedure codes 97153, 9754, 97155, and 97158. Billed units cannot exceed 32 units per day. Failure to submit 32 units or less per day could result in claims being denied or rejected.
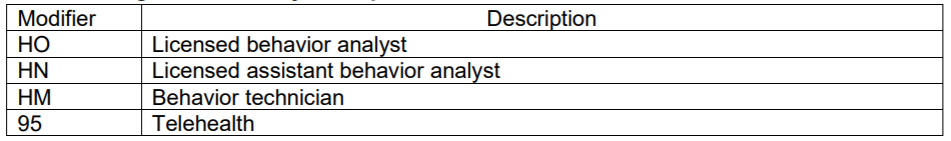
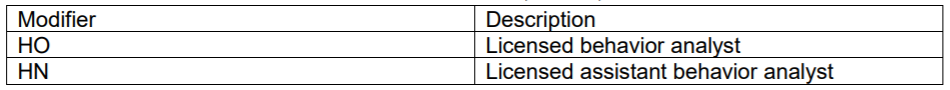
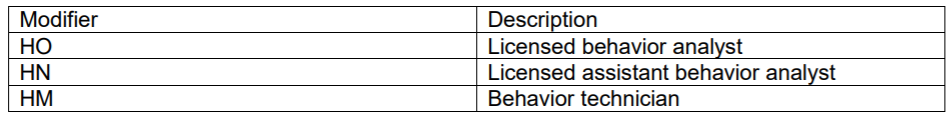
The following modifiers may be required for ABA services:
For clients who are birth through 20 years of age, the limitations listed below may be exceeded with evidence of medical necessity.
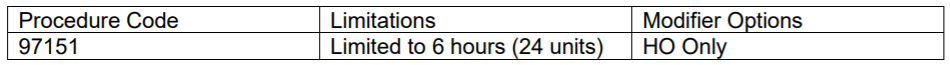
ABA – Initial Evaluation
ABA Re-evaluation
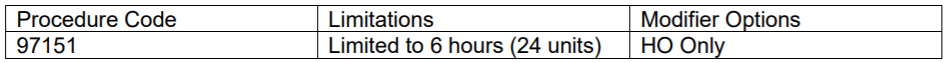
Procedure code 97151 is intended for conducting and reporting initial evaluations and treatment plans as well as re-evaluations by the LBA once every 180 days.
Procedure code 97151 will be authorized for up to 24 units (six hours) for the initial request of ABA services to complete an initial ABA evaluation and develop a treatment plan, to include data analysis and report writing.
Procedure code 97151 must be used within 30 calendar days of the first date of service for procedure code 97151 and is not reimbursable unless evaluation was submitted for authorization of payment.
Procedure code 97151 is eligible for reimbursement upon submission and approval of completed evaluation or re-evaluation. After the initial evaluation, procedure code 97151 will be authorized for up to 24 units (six hours) for re-evaluations for every subsequent authorization.
Failure to submit the correct modifier could result in claims being denied or rejected.
Modifiers – Evaluation and Re-evaluation Procedure Code 97151:
Procedure Codes – ABA Services (Individual Treatment)
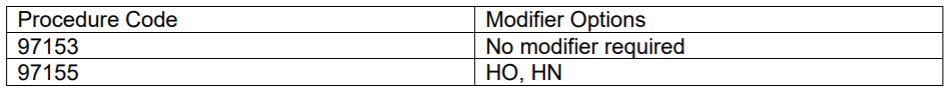
Procedure code 97155 is used by LBA (or as delegated to an LaBA) for direct one-on-one time with one child/youth to develop a new or modified protocol.
Procedure code 97155 may also be used to demonstrate a new or modified protocol to a BT, LaBA, and/or parents/caregivers with the child/youth with ASD present. The focus of this code is the skilled determination to make an addition or change to the protocol.
Procedure code 97155 may be used when directly supervising the BT or LaBA while working directly with the child/youth.
Either procedure code 97153 or 97155 may be used to request total hours of direct individual ABA treatment for the authorization period. Providers may then bill the code that reflects the treatment delivered.
Procedure Codes – ABA Group Treatment Services
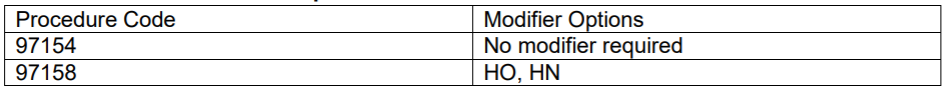
Procedure code 97154 is intended to be used for direct group ABA services delivered per ABA treatment plan protocol to the child/youth.
Procedure code 97154 designates a service of the complexity level appropriate for the delivery by a BT.
A group includes at least 2 patients but no more than 8.
Procedure code 97158 is used by LBA (or as delegated to an LaBA) for direct group time to develop a new or modified group treatment protocol.
Either procedure code 97154 or 97158 may be used to request total hours of direct group ABA treatment for the authorization period. Providers may then bill the code that reflects the treatment delivered.
Procedure Code – ABA Parent/Caregiver/Family Education and Training Services
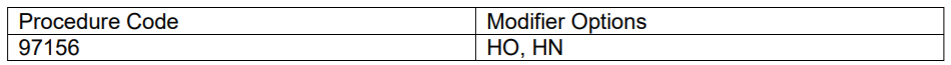
Procedure code 97156 is used by the LBA (or as delegated to an LaBA) for guiding the parents/caregivers (with or without the child/youth with ASD present) to utilize the ABA treatment plan protocols to reinforce adaptive behaviors for durability and generalizability. LBAs may delegate parent/caregiver teaching to LaBAs working under their supervision. LaBAs may not deliver services remotely via telehealth.
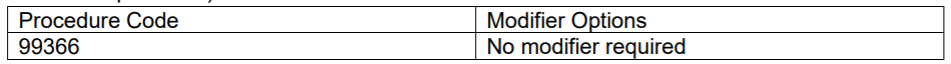
Procedure Code – Interdisciplinary Team Meetings (attended by qualified non-physician healthcare providers):
Modifiers – ABA Services Procedure Codes 97155, 97156, and 97158:
Modifiers – Behavior Technician Level Services- Procedure Codes 97153 and 97154 (modifiers for information purposes):
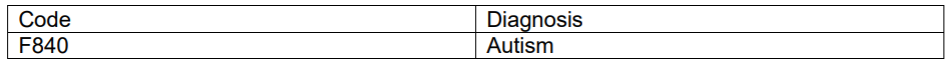
Reimbursement for procedure code 99366 is limited to the following diagnosis code and is contingent upon prior authorization of ABA evaluation, reevaluation, or treatment services:
Diagnosis Code
- Texas Medicaid will not reimburse multiple ABA providers during one ABA session with a child/youth when more than one ABA provider is present (concurrent billing).
- Concurrent billing is excluded except when the family and the child/youth with ASD are receiving separate services and the child/youth is not present in the family session.
- Texas Medicaid will not reimburse for ABA treatment services when the child/youth and/or family is not present and engaged in a therapeutic relationship.
- Reimbursement for covered ABA procedure codes are for the direct service time. Pre and post work for the session are not reimbursed separately. Separate reimbursement for treatment planning, note documentation, report writing, or updating of charts and data sheet is prohibited (other than what is allowable under procedure code 97151).
Some service delivery to children/youth and/or parents/caregivers may be delivered remotely. It is the LBA’s responsibility to ensure that remotely delivered telehealth services are within scope of practice, not contraindicated for the child/youth, family, or particular situation, are clinically appropriate and effective, and in compliance with Texas licensure and standards for telehealth as well as follow all Medicaid, Texas Health Steps-CCP and this policy’s requirements. ABA evaluation and treatment services may only be delivered via telehealth using synchronous audio-visual technology or a similar technology.
The following procedure codes may be delivered via telehealth:
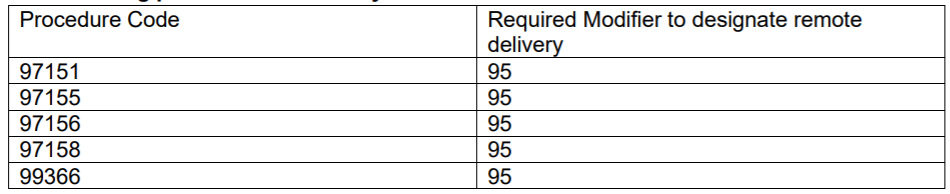
LaBAs and RBTs may not deliver any service remotely.
Reimbursable remote delivery services must include synchronous audiovisual interaction between the distant site provider and the child/youth or parent/caregiver in another location.
Method for Counting Minutes for Timed Procedure Codes in 15-Minute Units
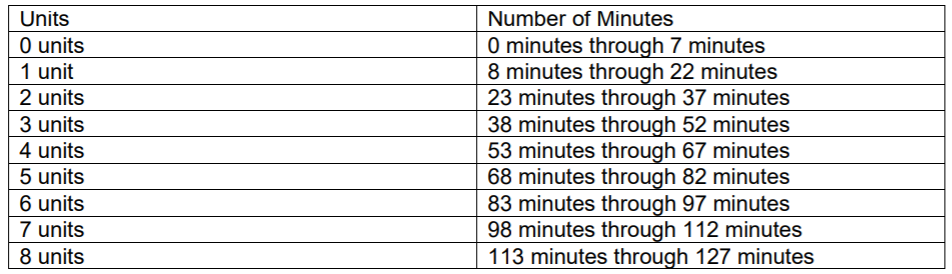
All claims for reimbursement of procedure codes paid in 15-minute increments are based on the actual amount of billable time associated with the service. For those services for which the unit of service is 15 minutes (1 unit = 15 minutes), partial units should be rounded up or down to the nearest quarter hour.
To calculate billing units, count the total number of billable minutes for the calendar day for the client, and divide by 15 to convert to billable units of service. If the total billable minutes are not divisible by 15, the minutes are converted to one unit of service if they are greater than seven and converted to zero units of service if they are seven or fewer minutes.
For example, 68 total billable minutes/15 = 4 units + 8 minutes. Since the 8 minutes are more than 7 minutes, those 8 minutes are converted to one unit. Therefore, 68 total billable minutes = 5 units of service.
Counting Minutes for Timed Procedure Codes -Time intervals for 1 through 8 units are as follows:
Direct treatment for the child/youth is limited to a total of 8 hours per day, inclusive of procedure codes 97153, 9754, 97155, and 97158. Billed units cannot exceed 32 units per day.
Providers must follow these billing guidelines when providing Autism Services, to include Applied Behavior Analysis (ABA) evaluation and treatment.
https://www.tmhp.com/news/2021-07-30-hhsc-release-autism-services-benefits-effective-february-1-
2022
https://www.tmhp.com/sites/default/files/file-library/medicaid/autism-services-medicaid-draft-june2021.pdf
For additional information, please contact the Provider Relations Department at (210) 358-6294 or by email at ProviderRelations@CFHP.com.