Who can be a CPW (Children and Pregnant Women) Provider?
A Registered Nurse (RN) with an associate’s, bachelor’s, or advanced degree in nursing, whose license is not temporary or provisional in nature. The RN must attend and complete Health and Human Services Commission (HHSC) Case Management Training.
NOTE: An RN with an associate’s degree in nursing must also possess two years of cumulative, paid, full-time work experience or two years of supervised, full-time educational internship/practicum experience in the last ten years with children, up to age 21, and/or pregnant women. Experience must include assessing the psychological and health needs of and making community referrals for these populations.
A Licensed Social Worker (LSW) with licensure appropriate to practice, including the practice of Independent Social Work, and who license is not temporary or provisional in nature. The LSW must attend and complete HHSC Management Training.
Medicaid-enrolled CPW providers who render Texas Medicaid CPW services as an individual provider or as a performing provider with a group are responsible for complying with all Texas Medicaid requirements and provider responsibilities. CPW provider responsibilities include timely submission of appropriate and accurate forms and information, accurate billing to the extent that the CPW provider has responsibility for billing, licensing, registration, and certification.
How do I enroll in Texas Medicaid to provide Medicaid CPW services?
A group or a case manager must obtain an individual National Provider Identifier (NPI) regardless of whether they are enrolling in Texas Medicaid as an individual or a performing provider with a group. If the group, individual, or performing provider already has an NPI, they must have a case management taxonomy associated with their NPI.
To enroll in Texas Medicaid as a group, individual or performing CPW provider, the provider must:
- Submit an application to HHSC and obtain an HHSC approval letter. To learn about steps to start the process, email askCM@hhs.texas.gov
- Complete the HHSC Case Management Training before enrolling as a Medicaid CPW provider. All case managers must attend this training.
- Obtain the appropriate NPI from the Center for Medicare and Medicaid Services (CMS).
Note: After September 1, 2022, a provider must complete the HHSC Case Management Training before starting the CPW provider enrollment process through Texas Medicaid and Healthcare Partnership (TMHP).
You can click on the link below for any additional information regarding the enrollment process. https://www.tmhp.com/sites/default/files/file-library/medicaid/CPW-Provider-Enrollment-QRG.pdf
How do I start the enrollment process through TMHP?
After obtaining an NPI, visit the Provider Enrollment page and the How to Apply for Enrollment page located on the TMHP website (TMHP.com) to begin enrollment in Texas Medicaid.
Providers may want to reference the general TMHP Step-by Step-Guide for Provider Enrollment page to enroll (https://www.tmhp.com/sites/default/files/file-library/topics/provider- enrollment/provider-enrollment-tools-QRG.pdf).
The enrollment process may take up to 30 business days to complete after the provider submits an enrollment application with no deficiencies. Performing providers must hold a current and active license from their respective licensing board and meet all other eligibility requirements.
Note: When enrolling, check the box to enroll as a Case Management for Children and Pregnant Women provider. Do not check enrollment as a CCP Social Worker.
Enroll as HHSC approved you. If HHSC approved you as a group, click Group Enrollment. If HHSC approved you as an individual provider, click Individual Provider. This will be designated on your HHSC approval letter. For help completing the enrollment application or general information regarding provider enrollment, call the TMHP Contact Center at 800-925-9126, Option 3. The Contact Center is open from 7:00 a.m. to 7:00 p.m., Central Time.
How do I contract and credential with a Texas Medicaid Managed Care Organization (MCO)?
After enrollment in Texas Medicaid through TMHP, CPW providers need to reach out to individual MCOs to contract and become credentialed to provide CPW services for the MCO.
To find the MCOs in your area, review the HHSC’s map of managed care service delivery areas, (https://www.hhs.texas.gov/sites/default/files/documents/services/health/medicaid- chip/programs/managed-care-service-areas-map.pdf).
If Community First Health Plans, Inc. (Community First), is the MCO in your area, please click on the link to begin the process. Staff will contact you directly to advise of next steps.
NOTE: CPW services are NOT a Children’s Health Insurance Program (CHIP) benefit.
How do I bill an MCO once I am contracted and credentialed?
To be eligible for services, a person must:
- Be eligible for Texas Medicaid.
- Be a pregnant woman who has a high-risk condition or a child (birth through 20 years of age) who has a health condition or health risk.
- Need assistance in gaining access to necessary medical, social, educational, and other services related to their health condition, health risk, or high-risk condition.
- Want to receive case management services.
Pregnant women who have a high-risk condition are defined as those who have a medical or psychosocial condition that places them and their fetus at a greater than average risk for complications, either during pregnancy, delivery, or following birth. Children with a health condition are defined as children who have a health condition or health risk or children who have or are at risk for a medical condition, illness, injury, or disability that results in the limitation of function, activities, or social roles in comparison with healthy same-age peers in the general areas of physical, cognitive, emotional, or social growth and development.
Case Management for Children and Pregnant Women services are limited to one contact per day per person. Additional provider contacts on the same day are denied as part of another service rendered on the same day.
Procedure code G9012 is to be used for all Case Management for Children and Pregnant Women services. Modifiers are used to identify which service component is provided.
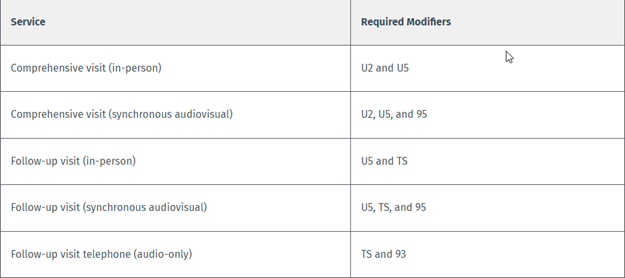
Providers must adhere to Case Management for Children and Pregnant Women program rules, policies, and procedures. Claims submitted with incorrect modifiers or incorrect CPT codes will be denied.
NOTE: Case Management for Children and Pregnant Women providers are not required to file claims with other health insurance before filing with Medicaid. Case Management for Children and Pregnant Women services are not billable when a person is an inpatient at a hospital or other treatment facility. Reimbursement will be denied for services rendered by providers who have not been approved by HHSC.
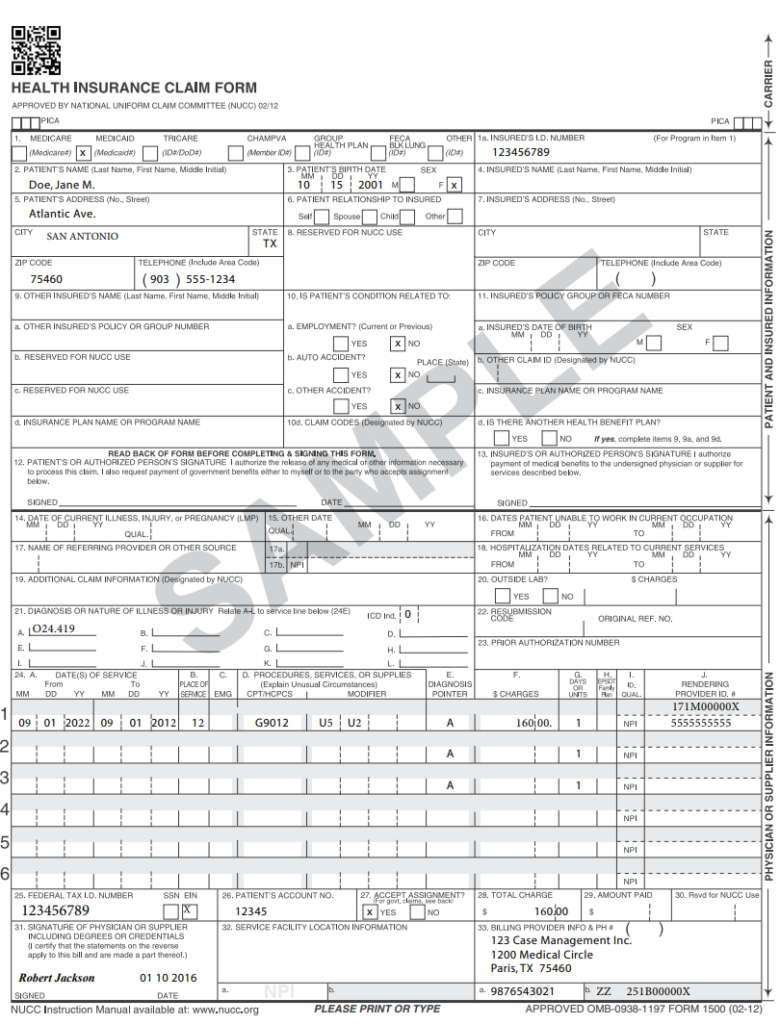
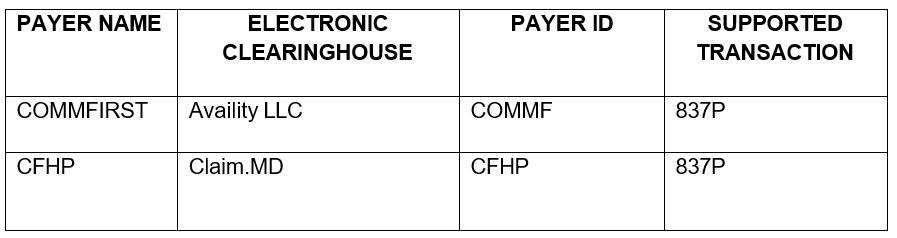
Claim submissions must be filed to Community First within 95 days from the date of service and can be submitted in various ways. Below are clearinghouses Community First currently receives claims from. We have included a sample claim form to simply the filing process.
Are Prior Authorizations Required?
- Prior authorizations are not required for CPW Services.
- Members may self-refer to a CPW network provider. Provider referrals for CPW services are not required.
- If provider is out of network, Community First will provide continuity of care for 90 days until Member can be transferred to another participating provider or Network Management may contract with said out of network Provider.
Contact Information:
Community First has a dedicated email and phone number to help providers answer questions related to CPW. Please email chelp@cfhp.com or call 210-413-8649.
For general inquires or assistance, email ProviderRelations@cfhp.com or call 210-358-6294.